Key Takeaways
- Agentic Process Automation surpasses traditional automation by employing autonomous AI agents that learn, adapt, and act independently without human intervention, enhancing decision-making in complex environments.
- APA optimizes healthcare claims by automating repetitive tasks such as eligibility checks, coding, and adjudication, reducing delays, increasing accuracy, and improving provider-patient satisfaction.
- APA enables seamless integration across the claims lifecycle—from data ingestion to reimbursement—reducing manual effort, minimizing errors, and boosting operational efficiency.
- With machine learning, APA identifies suspicious patterns in claims data, helping to prevent fraud, ensure compliance, and maintain trust in healthcare reimbursement systems.
- The future of APA includes predictive analytics, conversational AI, and blockchain, enabling real-time interaction, proactive error prevention, and transparent, secure claims tracking.
One industry that is going above and beyond to improve efficiency, enhance productivity, and patient experiences is the healthcare sector. Nevertheless, one area where all of these goals play a vital role is claims processing. Agentic process automation helps firms by offering a feasible solution by utilizing innovative agents, automation, and AI.
Most healthcare firms are unaware that APA is more than just traditional automation. This is because it utilizes AI-powered agents to operate independently. No human intervention is needed at all. Additionally, APA has the expertise to review all medical documents for errors. This way, medical experts can ensure that the records contain the correct information.
Furthermore, APA can inform medical experts if any information is missing in the papers. However, if you are a business that wants to adapt APA, it is essential to follow all the rules and regulations set by the insurance firms. Only then will there be less manual work, and no delays will be made.
APA also helps healthcare settings process claims accurately and efficiently, reducing errors and saving time. This means there are no delays, fewer claims are rejected, and payments are made faster. Patients get access to top-notch service with their insurance claims. On the other hand, healthcare providers and insurance companies benefit from improved cash flow. Hence, to utilize agentic process automation, healthcare firms need to select suitable processes that are suitable for automation. Additionally, they should integrate the system with their existing tools and ensure that agents are trained to utilize real data. There might be some challenges on the way, but the outcomes are worth the effort.
Also read: Agentic AI in Healthcare: Beyond Chatbots to Clinical Decision Support.
What is Agentic Process Automation
Agentic process automation refers to the use of autonomous AI agents that can perceive their environment, make decisions, and take actions to complete tasks with minimal human intervention. Unlike traditional robotic process automation, which follows predefined rules and workflows, APA agents can learn, adapt, and operate in dynamic environments.
In simpler terms, APA combines advanced AI technologies, such as machine learning, natural language processing, and decision intelligence, with automation tools. These agents simulate human-like behavior to perform complex tasks, such as interpreting documents, making decisions, and interacting with multiple systems in real-time.
Why Focus on Healthcare Claims Processing?
Claims processing is a vital function in the healthcare system. It ensures that healthcare providers are reimbursed for the services they deliver and that patients’ insurance benefits are applied correctly. However, this process is often slow, error-prone, and heavily reliant on manual work. A single claim can pass through several stages, including eligibility verification, coding and documentation review, compliance checks, approval workflows, and ultimately, payment or reimbursement. Each of these steps can involve different systems, departments, and regulations, increasing the likelihood of delays or errors.
Due to this complexity and volume, claims processing presents a prime area for improvement through Agentic Process Automation (APA). APA uses a combination of artificial intelligence (AI), automation, and intelligent agents that can perform tasks independently, understand patterns, and make decisions based on data. This makes it especially valuable in environments such as claims processing, where repetitive tasks and decision-making based on established rules are the norm.
By integrating APA into the claims lifecycle, healthcare organizations can significantly reduce the amount of manual effort required. Intelligent agents can extract data from documents, validate it against payer rules, check for coding errors, verify patient eligibility, and even flag suspicious claims for further review. These agents work 24/7 and do not experience fatigue, which helps to speed up processing times and reduce backlogs.
Faster claims processing has a direct impact on both healthcare providers and patients. Providers receive payment more quickly, which improves their cash flow and enables them to focus more on delivering care rather than managing paperwork. Patients benefit from fewer claim denials and quicker resolution of billing issues, resulting in improved overall satisfaction. Moreover, APA helps reduce administrative costs by minimizing the need for manual reviews and rework. It also improves accuracy by reducing human errors, which are a common cause of claim rejections or payment delays.
In a healthcare environment where every dollar and every minute counts, automating and optimizing claims processing is no longer optional—it’s necessary. APA offers an innovative and scalable way to handle claims more efficiently, ensuring that both financial and operational goals are met while maintaining a positive experience for patients and providers alike.
Key Components of APA in Healthcare Claims Processing
Agentic process automation introduces a smarter, faster, and more accurate approach to handling healthcare claims. By leveraging artificial intelligence, automation, and intelligent agents, APA addresses the key stages of the claims lifecycle. Below are the major components of APA and how they help streamline healthcare claims processing:
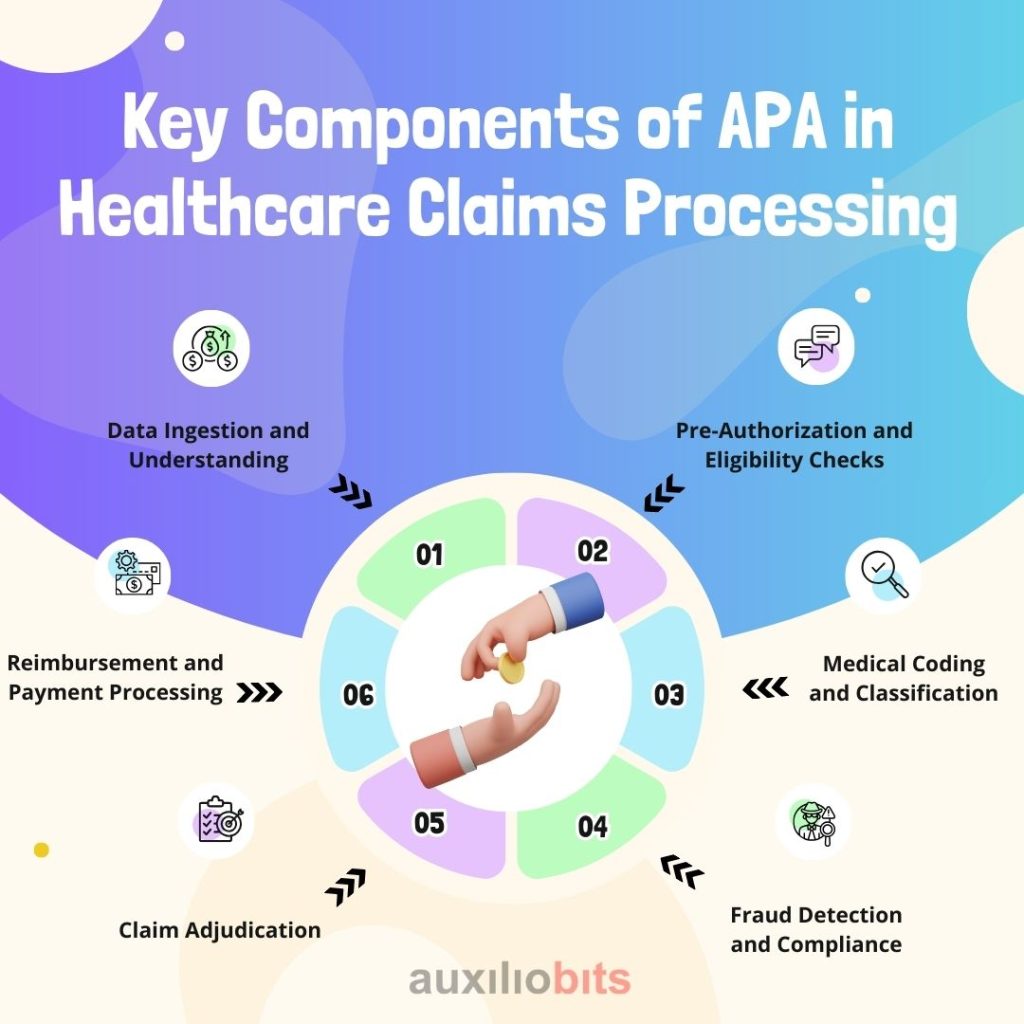
1. Data Ingestion and Understanding
Healthcare data is diverse and often unstructured, coming from Electronic Health Records (EHRs), scanned documents, claim forms, emails, and PDFs. APA agents utilize technologies such as Optical Character Recognition (OCR) to convert scanned or handwritten content into machine-readable formats. Combined with Natural Language Processing (NLP), the agents can understand medical language, extract relevant information such as patient details, diagnosis codes, and treatment dates, and organize the data for further processing. This eliminates the need for manual data entry and reduces the chances of human error.
2. Pre-Authorization and Eligibility Checks
Before treatments are carried out, verifying insurance eligibility and obtaining pre-authorization are crucial to ensure coverage. APA agents can connect with payer systems through secure APIs and verify patient insurance status in real-time. They can also handle pre-authorization requests by submitting necessary documentation and following up with payers. Automating this step helps prevent claim denials due to eligibility issues and reduces the time staff spend on phone calls and emails.
3. Medical Coding and Classification
Accurate coding is crucial for claims to be accepted and processed efficiently. Using AI and historical data, APA agents can automatically analyze clinical notes and treatment descriptions to assign the correct ICD-10 and CPT codes. These agents are trained on a wide range of medical cases and can adapt over time, learning from feedback to improve accuracy. This ensures that the coding is consistent, complete, and compliant with payer requirements.
4. Fraud Detection and Compliance
Claims fraud and regulatory compliance are ongoing challenges in healthcare. APA systems are equipped with machine learning models that analyze historical data to identify unusual patterns or inconsistencies. For example, they can flag claims with unusually high charges, duplicate submissions, or treatments not typically associated with a diagnosis. These checks support fraud prevention and help ensure compliance with healthcare laws and standards, including HIPAA.
5. Claim Adjudication
One of the most critical steps in claims processing is adjudication, which involves determining whether a claim should be approved or denied. APA agents can evaluate claims based on the coverage terms, prior authorizations, coding accuracy, and payer rules. They can make real-time decisions or flag complex cases for further review by humans. This significantly accelerates the adjudication process and enhances accuracy.
6. Reimbursement and Payment Processing
After a claim is approved, APA agents can trigger automated payment processes. They can issue payment instructions, update patient accounts, and manage entries in financial systems such as ERP platforms. This reduces delays in reimbursements, ensures accurate payment reconciliation, and helps healthcare providers maintain healthy cash flow.
Together, these components make APA a powerful tool for transforming healthcare claims processing. By automating end-to-end workflows, APA not only saves time and money but also improves accuracy, compliance, and patient satisfaction.
The Future of Claims Processing
As artificial intelligence continues to advance, the future of healthcare claims processing is set to become more intelligent, automated, and patient-centric. Agentic Process Automation (APA) systems are evolving rapidly, and in the coming years, we can expect these systems to take on more complex tasks with even greater autonomy. This shift will not only reduce administrative burdens but also improve transparency, accuracy, and the overall experience for patients and healthcare providers.
One promising area of development is the use of Conversational AI agents. These intelligent virtual assistants will be capable of interacting directly with patients, answering common questions related to claim status, outstanding balances, or denied claims. Instead of waiting on hold or navigating complex web portals, patients will be able to get real-time answers through voice or chat interfaces. This will improve communication, reduce support workloads, and increase patient satisfaction.
Another exciting possibility is the application of predictive analytics in the claims process. APA systems will be able to analyze historical claims data to identify patterns that often lead to denials. By doing this early in the process, the system can alert healthcare providers about potential issues before the claim is submitted. This allows teams to correct errors or provide additional documentation, improving first-pass acceptance rates and reducing delays in reimbursement.
Blockchain integration is also gaining attention as a future component of the claims processing process. Blockchain technology provides a secure and decentralized method for storing and sharing data. By using blockchain, claims can be tracked transparently from submission to settlement. All parties—patients, providers, and payers—would have access to a single, accurate version of the truth, thereby reducing disputes, fraud, and administrative costs. Smart contracts on the blockchain could even trigger automatic payments once claim conditions are met.
As APA continues to evolve, healthcare organizations that invest in these technologies early will gain a significant advantage. By automating and optimizing claims workflows, they can reduce costs, expedite processing, and deliver better service to patients. In a competitive healthcare environment, embracing the future of APA is not just about efficiency—it’s about creating a system that is more responsive, transparent, and aligned with the needs of modern patients and providers.
Conclusion
Agentic Process Automation is revolutionizing healthcare claims processing by replacing manual, repetitive tasks with intelligent, self-learning agents. From improving efficiency and accuracy to enhancing patient and provider experiences, APA offers transformative potential. While challenges exist, with the proper planning and execution, healthcare organizations can lay the groundwork for a more efficient and intelligent future.
Now is the time to explore APA and bring next-level automation into your claims processing ecosystem.