
Key Takeaways
- Synthetic data enables safe AI training in healthcare by mimicking real datasets without compromising patient privacy, ensuring compliance with regulations like HIPAA and GDPR.
- Synthetic data solves critical data access issues by simulating diverse clinical scenarios, rare diseases, and patient groups, supporting the development of robust and unbiased AI models.
- Techniques like GANs, VAEs, and diffusion models are essential tools for generating realistic synthetic data in various formats—EHRs, medical images, clinical notes, and genomics.
- Synthetic data supports ethical AI validation by allowing safe testing in simulated environments, eliminating risks associated with using sensitive real-world patient information.
- Widespread adoption requires responsible implementation, including careful technique selection, ethical oversight, and adherence to legal frameworks for trustworthy healthcare AI innovation.
Since artificial intelligence has been utilized, the healthcare industry has experienced a significant digital revolution. AI is increasingly introducing remarkable innovations in the industry. From improving diagnostics to ensuring patients get timely treatment, AI has made it easier for healthcare professionals to prioritize patient care. In addition, patients no longer have to wait in long queues for an appointment. Nevertheless, the effectiveness of AI is dependent on one central element: access to vast volumes of data.
The professionals in the healthcare sector generate huge amounts of data on a regular basis. However, when they use this data for AI development, there are several challenges on the way. Strict privacy regulations such as HIPAA in the USA and GDPR in Europe impose limits on how professionals should access patient data. Apart from this, practical problems such as incomplete or unstructured records and insufficiently labeled datasets often hinder the development of robots’ AI solutions. All of these challenges slow innovation and give rise to models that underperform.
To avoid such challenges, synthetic data generation has come to the rescue.
Also read: Building Centers of Excellence for Enterprise-Wide Implementation
What is Synthetic Data in Healthcare?
Synthetic data refers to any data that is artificially generated. Instead of gathering data from people or real-world events, synthetic data is created with the help of machine learning algorithms, simulations, and statistical models. However, firms need to understand that synthetic data is not a copy of real data. It is a new dataset that mimics the characteristics of the original data while ensuring that all the sensitive information is protected.
In the healthcare sector, synthetic data can take several forms. It all depends on the source type and application:
1. Electronic Health Records
This consists of all the structured data, including medical histories, medication prescriptions, and patient demographics. Synthetic EHRs can be utilized by experts to make sure that all the machine learning models are trained without exposing real patient details. This helps them test healthcare applications, validate AI algorithms, and conduct epidemiological studies while making sure that all the rules and regulations are followed.
2. Medical Images
Synthetic medical imaging data, including CT scans, ultrasounds, X-rays, and MRIs, are generated by utilizing technologies like generative adversarial networks. These synthetic images replicate the visual patterns of real scans. They are further used to train diagnostic models, test imaging software, and develop image recognition tools.
3. Clinical Notes
These are unstructured textual data that capture interactions between doctors and patients. Natural language processing (NLP) models can be trained on synthetic clinical notes to identify patterns, extract medical entities, or build virtual assistants. Synthetic clinical notes are useful for developing AI solutions in medical documentation and decision support without risking the disclosure of sensitive information.
4. Sensor/IoT Data
In modern healthcare, wearable devices and IoT systems generate streams of real-time data such as heart rate, temperature, blood oxygen levels, and movement patterns. Synthetic time-series data can simulate these measurements, allowing developers to test remote monitoring systems and predictive health algorithms in a privacy-preserving manner.
5. Genomics and Proteomics Data
These high-dimensional datasets involve DNA, RNA, and protein sequences. Synthetic omics data enables research in precision medicine, genetic disorder prediction, and drug discovery without accessing real patient genomes. Machine learning models can simulate synthetic sequences that mirror genetic variations and biological markers found in real populations.
Overall, synthetic data in healthcare provides a privacy-respecting, scalable, and cost-effective solution for research, development, and training of AI models. It accelerates innovation while safeguarding patient confidentiality and complying with data protection laws.
Why Use Synthetic Data in Healthcare?
Synthetic data is increasingly gaining traction in healthcare because it addresses several critical challenges associated with real-world medical data. These challenges include strict privacy regulations, limited access to large and diverse datasets, and the need for safe and ethical development of AI systems. Below are the key reasons for using synthetic data in healthcare, expanded in detail:
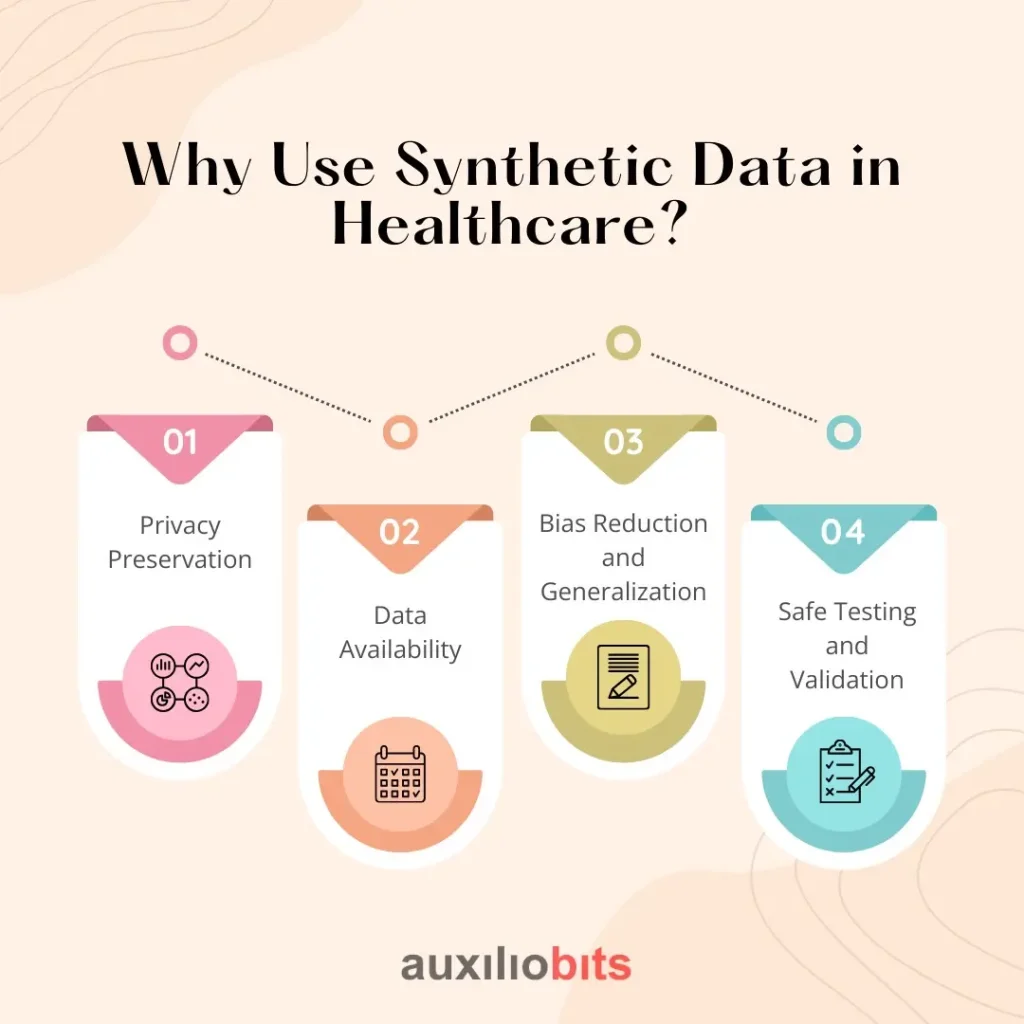
1. Privacy Preservation
Healthcare data is among the most sensitive types of personal information, protected by stringent regulations such as HIPAA (Health Insurance Portability and Accountability Act), GDPR (General Data Protection Regulation) and HITECH (Health Information Technology for Economic and Clinical Health Act). These laws ensure that patient data remains confidential and secure. However, they also create barriers to data sharing and AI development. Synthetic data helps resolve this tension by offering privacy-preserving alternatives. Because it is generated without directly replicating any individual’s records, a well-designed synthetic dataset contains no personally identifiable information (PII). This makes them safe to use for research, training, and model development without the need for complex anonymization processes or legal compliance hurdles.
2. Data Availability
High-quality, annotated medical data is scarce due to the complexity of data collection and the sensitivity surrounding patient information. This scarcity becomes a major roadblock for training effective AI models, which typically require vast amounts of diverse data. Synthetic data offers a solution by augmenting existing real datasets or simulating entire datasets from scratch. It can replicate typical clinical scenarios or generate rare events, such as uncommon diseases or complications, which are difficult to collect in sufficient quantities. This makes synthetic data invaluable for enhancing training data diversity and supporting the development of robust, generalizable AI systems.
3. Bias Reduction and Generalization
Real-world healthcare datasets often contain demographic or clinical biases due to underrepresentation of certain populations, such as racial minorities, elderly patients, or those with rare conditions. These biases can lead to AI systems that perform well on majority groups but poorly on others, potentially resulting in inequitable care. Synthetic data generation allows for greater control over the statistical properties of the data, including population balance. Developers can simulate datasets that are more representative of diverse patient groups, which helps reduce algorithmic bias and ensures more equitable healthcare outcomes
4. Safe Testing and Validation
Before deploying AI systems in clinical environments, it’s essential to test them thoroughly to ensure they perform accurately and safely. Using real patient data for testing poses ethical and legal challenges. Synthetic data provides a safe and compliant environment for prototyping and validating AI models. It allows developers to simulate various clinical scenarios—normal and edge cases alike—without any risk of harming real patients or violating data usage policies.
Synthetic Data Generation Techniques for Healthcare
Generating synthetic data in healthcare requires a careful balance between realism, privacy, and utility. Various techniques are employed to produce synthetic medical data depending on the type—structured records, unstructured text, or images—and the desired outcomes. Below are five key approaches used to generate synthetic healthcare data, each with unique strengths and applications.
1. Generative Adversarial Networks (GANs)
GANs are one of the most powerful and popular techniques for generating high-fidelity synthetic data. A GAN is composed of two neural networks—a generator, which creates synthetic data, and a discriminator, which evaluates its authenticity. The networks train in a loop where the generator learns to fool the discriminator, resulting in increasingly realistic outputs over time.
In healthcare, GANs are used extensively for generating medical images (like MRI or CT scans), structured tabular data (such as electronic health records), and rare disease simulations. A notable example is MedGAN, specifically developed to generate synthetic EHR data while preserving the statistical relationships between medical codes and patient histories.
Use Cases: Synthetic MRI and CT scans, dermatology images (e.g., skin lesions), simulated patient records for AI training.
2. Variational Autoencoders (VAEs)
VAEs are another deep generative model that operates by encoding real data into a compressed latent space and then decoding it back into synthetic samples. VAEs tend to be more stable during training than GANs and offer greater control over the generated data through the latent variables.
They are particularly effective for synthesizing EHR data, where controlled variations and sampling from the latent space can simulate disease progression, medication responses, or anomalies in patient profiles.
Use Cases: Generation of synthetic EHRs, simulation of chronic disease progression, anomaly detection in health monitoring systems.
3. Simulation-Based Approaches
These involve the use of biological, epidemiological, or operational models to simulate healthcare scenarios. For example, agent-based models can mimic the movement and interactions of patients and staff in a hospital, while epidemiological models can simulate the spread of infectious diseases.
These methods are grounded in domain expertise and often used for policy simulation, resource planning, and capacity modeling rather than deep learning training.
Use Cases: ICU patient flow simulation, pandemic modeling, hospital bed occupancy forecasting.
4. Rule-Based and Programmatic Generation
This technique relies on clinical rules, templates, or domain knowledge to produce synthetic data. It is commonly used for structured tasks like lab test generation or for natural language processing (NLP) applications such as synthetic clinical note creation.
Rule-based systems are particularly valuable when interpretability and traceability are important or when datasets are needed to train dialogue systems and medical chatbots.
Use Cases: Generating synthetic progress notes, pathology reports, chatbot conversations, and lab results based on clinical standards.
5. Diffusion Models (Emerging)
Inspired by the success of models like DALL·E and Stable Diffusion in image generation, diffusion models are now being explored for medical imaging tasks. These models work by progressively refining random noise into detailed images, offering superior fidelity, diversity, and control compared to GANs.
Though still emerging, early research indicates diffusion models could outperform GANs in generating high-resolution radiological images while preserving critical diagnostic features.
Use Cases: Synthetic X-rays and pathology slides, enhancing data diversity for AI radiology tools.
Conclusion
Synthetic data stands at the forefront of AI innovation in healthcare, offering a pragmatic path to overcome privacy concerns and data scarcity. However, it’s not a silver bullet. Responsible use requires a thoughtful balance between technical rigor, ethical vigilance, and regulatory compliance.
As the healthcare sector increasingly embraces AI, the role of synthetic data will only expand. By investing in trustworthy generation techniques and rigorous governance, healthcare organizations can harness its full potential to unlock safer, fairer, and more intelligent health systems.








