
Key Takeaways
- Revenue leakage in healthcare is often invisible but costly, arising from errors in coding, registration, authorization, and claim submission processes.
- Automated Pre-Adjudication (APA) acts as a proactive audit system, catching issues like missing documents or incorrect coding before claims are submitted, significantly reducing denials.
- Business Intelligence Automation supercharges APA, offering predictive analytics, real-time payer policy tracking, and intelligent workflow orchestration to eliminate manual errors.
- APA and BI Automation together improve cash flow, increase collected revenue, lower admin costs, and enhance regulatory compliance, all while reducing staff workload.
- The future of healthcare revenue cycle management is predictive and autonomous, not reactive and manual. APA offers a scalable path toward financial resilience and better patient experiences.
Healthcare providers today face immense pressure to deliver quality care while maintaining financial stability. One of the biggest silent threats to a healthcare organization’s bottom line is revenue leakage. It’s like a slow, steady drip, eroding profits and hindering growth. But what if there were a powerful solution to plug these leaks and optimize your financial health? Enter Automated Pre-Adjudication (APA), a game-changer in healthcare revenue cycle management, powered by the intelligence of Business Intelligence Automation.
Also read: HyperAutomation in Healthcare Reducing Admin Burden with AI
What is Revenue Leakage, and Why is it a Big Deal in Healthcare?
Revenue leakage, in simple terms, is money that healthcare providers are rightfully owed but fail to collect. This can happen at various stages of the patient journey, from registration to claims submission and denial management. Think of it as a leaky faucet—a small drip doesn’t seem like much, but over time, it can waste gallons.
In healthcare, these “drips” can come from:
- Coding Errors: Incorrect or incomplete medical coding can result in underpayment or outright rejection.
- Registration Discrepancies: Inaccurate patient information, insurance details, or eligibility can cause delays and denials.
- Lack of Prior Authorization: Services rendered without necessary pre-approvals from payers often go unpaid.
- Inefficient Claims Processing: Manual errors, slow submissions, and a lack of timely follow-up on denied claims.
- Underutilized Contract Terms: Not fully leveraging negotiated rates with insurance companies.
- Duplicate Services: Unintentional billing for the same service multiple times.
The cumulative effect of these leakages can be substantial, impacting a healthcare organization’s ability to invest in new technologies, attract top talent, and ultimately, provide better patient care.
Introducing APA: Your Revenue Leakage Plug
Automated Pre-Adjudication (APA) is a sophisticated technology that intervenes before a claim is even submitted to the payer. It acts as a proactive audit, meticulously reviewing claims for potential errors, discrepancies, and missing information that could lead to denials or underpayments.
Instead of waiting for a claim to be rejected and then scrambling to fix it, APA identifies these issues upfront. This includes:
- Verifying patient eligibility and benefits.
- Checking for proper coding and medical necessity.
- Ensuring all required documentation is present.
- Identifying potential policy conflicts or coverage limitations.
- Cross-referencing against payer-specific rules and guidelines.
By catching these issues before submission, APA significantly reduces the chances of denials, accelerates payment cycles, and minimizes the administrative burden associated with rework.
The Powerhouse Behind APA: Business Intelligence Automation
While APA is powerful on its own, its true potential is unlocked when seamlessly integrated with Business Intelligence Automation. This is where data transforms into actionable insights, and manual processes become intelligent, automated workflows.
Business Intelligence (BI), at its core, is about collecting, analyzing, and presenting data to help organizations make informed decisions. When you add Automation to BI, you get a system that not only understands your data but also acts on it autonomously.
Here’s how Business Intelligence Automation supercharges APA in reducing revenue leakage:
1. Automated Data Collection and Integration:
BI automation pulls data from various disparate systems – Electronic Health Records (EHR), practice management software, billing systems, and even payer portals. This eliminates manual data entry errors and ensures APA is working with the most up-to-date and comprehensive information.
2. Predictive Analytics for Denial Prevention:
Leveraging historical claims data and machine learning, Business Intelligence Automation can predict which claims are most likely to be denied and identify the reasons why. This allows APA to focus its efforts on high-risk claims, proactively addressing potential issues before they arise.
3. Real-time Insights into Payer Trends
BI automation continuously monitors payer rules, policy updates, and common reasons for denials. This real-time intelligence feeds directly into APA, ensuring that the pre-adjudication process is always aligned with the latest requirements, minimizing surprises.
4. Automated Workflow Optimization:
When APA identifies an issue, Business Intelligence Automation can trigger automated workflows. For example, if a prior authorization is missing, the system can automatically flag it, notify the relevant department, and even initiate the initial authorization request process.
5. Performance Monitoring and Continuous Improvement:
BI dashboards provide clear, real-time visibility into the effectiveness of APA. You can track denial rates, identify common leakage points, and measure the financial impact of your pre-adjudication efforts. This data-driven feedback loop allows for continuous optimization and refinement of your revenue cycle processes.
6. Reduced Manual Intervention and Human Error:
By automating data gathering, analysis, and initial corrective actions, Business Intelligence Automation significantly reduces the need for manual intervention, freeing up staff to focus on more complex tasks and further minimizing human errors that contribute to revenue leakage.
The Tangible Benefits: Why Every Healthcare Provider Needs This
Implementing APA, powered by Business Intelligence Automation, offers a multitude of benefits that directly impact your financial health and operational efficiency:
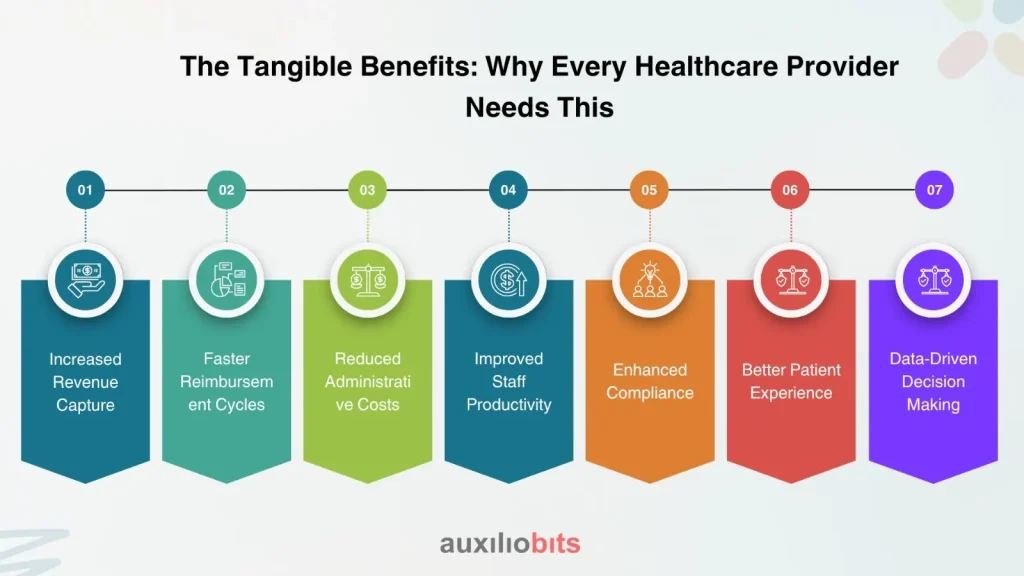
By proactively identifying and correcting errors, you can significantly reduce denials and underpayments, resulting in a direct increase in collected revenue.
Clean claims result in quicker processing by payers, leading to faster payments and improved cash flow.
Less time spent on denial management, appeals, and manual rework translates into substantial cost savings.
Your billing and coding teams can shift their focus from reactive problem-solving to proactive optimization and patient support.
Automated checks ensure adherence to ever-evolving coding guidelines, payer rules, and regulatory requirements, reducing the risk of audits and penalties.
A streamlined billing process with fewer surprises contributes to higher patient satisfaction.
The rich insights provided by Business Intelligence Automation empower leaders to make strategic decisions about staffing, services, and technology investments.
The Future of Healthcare Revenue Cycle Management
In an increasingly complex healthcare space, relying on outdated, manual processes for revenue cycle management is no longer a sustainable approach. Revenue leakage is a pervasive problem, but it’s not an unconquerable one.
Automated Pre-Adjudication (APA), supercharged by the power of Business Intelligence Automation, offers a robust, proactive, and intelligent solution. It’s about transforming your revenue cycle from a reactive firefighting exercise into a highly efficient, predictive, and profitable operation.
By embracing these advanced technologies, healthcare organizations can not only plug revenue leaks but also build a more resilient, financially sound future, ultimately allowing them to focus on what matters most: delivering exceptional patient care.
Is your healthcare organization ready to unlock the full potential of its revenue? Explore how Automated Pre-Adjudication and Business Intelligence Automation can revolutionize your financial health today.








