
Key Takeaways
- Agentic AI plans, acts, and learns—perfect for messy admin work.
- Admin overload directly harms patient outcomes and finances.
- High-ROI targets: eligibility checks, scheduling, follow-ups, and reporting.
- Track efficiency, financial, and clinical KPIs to prove Automation ROI.
- Start small, measure fast, and scale responsibly.
Community health centers, rural hospitals, and mobile clinics serve millions of people who might otherwise go without care. Yet these teams spend as much time on paperwork as they do with patients. Phone calls to confirm insurance, emails to schedule visits, and forms to report outcomes fill the day and drain energy. Agentic AI, a new generation of smart software agents, offers a way out. By handling the dull, repetitive pieces of the workflow, it gives doctors, nurses, and front-desk staff the gift of time. This blog explains what Agentic AI is, how it works in community health, and—most importantly—how you can measure Automation ROI in both dollars and healthier lives.
Also read: Agentic AI: The Future of Business Process Optimization
What Is Agentic AI?
Traditional automation follows strict scripts: “If A happens, then do B.” It is fast but brittle. Agentic AI takes a different path. An agentic system:
- Plans: It sets a goal (e.g., “verify insurance for tomorrow’s appointments”) and chooses the steps to reach it.
- Acts: It signs in to payer portals, scans emails, and enters data in the EHR—just like a human assistant.
- Learns: When a payer website changes or a claim is rejected, the agent adapts instead of failing.
- Collaborates: It can chat with staff, hand off tricky cases, and ask clarifying questions.
Under the hood, these capabilities come from large language models, process-mining insights, and secure API connections. Think of Agentic AI as a super-reliable colleague who never gets tired, forgets a step, or loses patience. Because it is goal-driven, not line-by-line driven, it thrives in community health’s messy, multi-system environment.
The State of Admin Work in Community Health
A 2024 HealthIT.gov survey showed that staff in small clinics spend 37 percent of their week on admin tasks—higher than in large hospital chains. Common pain points include:
- Patient intake: Paper forms are retyped into the EHR.
- Eligibility checks: Staff call Medicaid or use outdated web portals.
- Appointment reminders: Manual SMS or phone trees that often fail.
- Grant reporting: Quarterly spreadsheets emailed to funders.
- Referrals and follow-ups: Juggling fax, phone, and email to close the loop.
Each task on its own seems small, but together they can delay care, shrink revenue, and exhaust employees. Worse, clinics rarely have IT budgets for modern solutions. That is why a flexible, low-code agentic layer is so attractive—it overlays existing tools rather than replacing them.
Why Administrative Burden Matters for Patient Care?
Paperwork is not just a nuisance; it has real clinical consequences:
- Delayed visits: If insurance cannot be verified, schedulers push the appointment back. In chronic conditions, every day counts.
- Missed appointments: A forgotten reminder means wasted slots and untreated patients.
- Data gaps: Hand-typed notes may omit allergies, meds, or social-risk factors.
- Staff burnout: High turnover disrupts continuity of care and raises hiring costs.
- Financial leakage: Unfiled claims or missing documents reduce revenue—funds that could hire another nurse or buy vaccines.
By cutting the admin load, Agentic AI improves both clinical quality and financial stability. In other words, Automation ROI here equals healthier communities and stronger balance sheets.
How Agentic AI Can Help?
Below are five high-impact workflows where agentic automation shines:
a) Digital Patient Intake
An AI chatbot texts or emails a secure link before the visit. Patients enter demographics, symptoms, and insurance photos. The agent screens for missing fields, writes a FHIR-compliant intake note, and uploads it to the EHR. Staff review, not re‑type.
b) Smart Scheduling & No-Show Prevention
The agent scans open slots, matches them to patient preferences, and sends reminders in the patient’s language. If a patient replies, “Can’t make it,” the agent offers new times and fills the gap with someone on the waiting list, keeping utilization high.
c) Real-Time Insurance & Eligibility Checks
Minutes after an appointment is booked, the agent logs in to payer APIs, verifies coverage, and flags co-pay amounts. For rejected checks, it suggests sliding-fee options or self-pay plans, avoiding day-of-visit surprises.
d) Post-Visit Follow-Ups
Lab orders, prescription refills, and specialist referrals often stall. The agent tracks each step, nudges patients through SMS, and alerts nurses if deadlines slip—especially critical for diabetes, hypertension, and prenatal care.
e) Automated Grant & Quality Reporting
Federally Qualified Health Centers (FQHCs) file UDS reports and quality measures. The agent extracts data from the EHR, cleans it, fills templates, and submits through secure portals—cutting a two-week job to two hours.
Each workflow returns time, reduces errors, and touches revenue. The cumulative Automation ROI can exceed 300 percent within 12 months, based on real deployments in clinics of under 50 staff.
Three Real-World Use Cases
Use Case 1: Rural Clinic Eligibility Bot
- Setting: 12-bed clinic in Iowa; 70 percent Medicaid.
- Old way: Two clerks spent 14 hours/week on eligibility calls.
- Agent: Overnight, the bot bulk-verified upcoming patients and wrote results in the EHR.
- Results: Manual effort down 90 percent; $64,000 extra reimbursements per year.
- Automation ROI: Paid back in 3 months; clerks now handle outreach programs.
Use Case 2: Urban FQHC No-Show Reduction
- Setting: Five-site nonprofit in Detroit; 28 percent no‑show rate.
- Agent: Multilingual reminder agent with behavioral nudges (e.g., “Reply 1 to confirm”).
- Results: No-show rate dropped to 11 percent; monthly revenue up $45,000.
- Automation ROI: 5× in the first year; patient satisfaction scores jumped from 7.1 to 9.0.
Use Case 3: Diabetes Follow-Up in a Tribal Clinic
- Setting: Reservation clinic with high A1c levels.
- Old way: Nurses called patients weekly; many numbers were out of service.
- Agent: AI text + voice agent integrated with telehealth.
- Results: 78 percent of patients completed HbA1c tests on time (up from 32 percent); average A1c fell by 1.2 points in nine months.
- Automation ROI: Harder dollars to measure, but grant renewal credited the program as a key success factor.
These stories show that Agentic AI is not sci-fi; it is working now and generating both financial and human returns.
Measuring Automation ROI in Community Healthcare
ROI calculations in healthcare must balance money saved with lives improved. Build a simple dashboard with three buckets:
| Bucket | Example KPI | Why It Matters |
| Efficiency | Admin minutes saved per visit | Frees staff for higher‑value work |
| Financial | Net revenue gain per month | Funds care expansion |
| Clinical/Patient | No‑show rate; A1c improvement | Direct health impact |
Formula:
pgsql
CopyEdit
Automation ROI (%) = (Annual Benefit − Annual Cost) / Annual Cost × 100
Include:
- Hard dollars: Reduced overtime, extra claims collected, and fewer denied bills.
- Soft savings: Lower turnover, less temp staffing, and shorter waitlists.
- Outcome value: Better quality scores may unlock pay-for-performance bonuses and grants.
Tip: Track the baseline for at least one month before deploying an agent so improvements are clear and credible.
Challenges and Things to Watch Out For
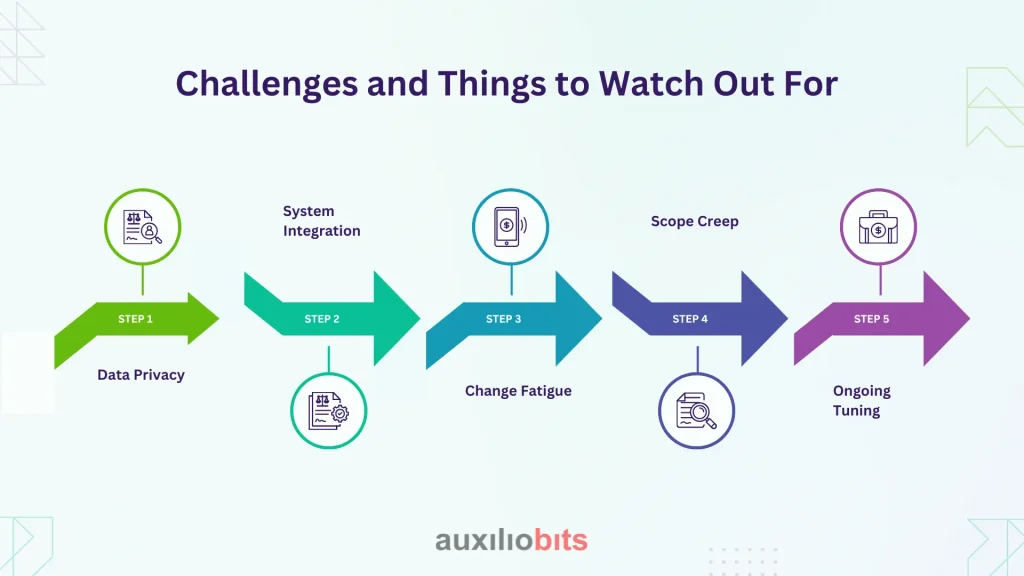
- Data Privacy: Ensure agents run inside a HIPAA-compliant environment. Use audit logs and role-based access.
- System Integration: Legacy EHRs may lack modern APIs. Pick vendors that provide robotic UI fallbacks or HL7 connectors.
- Change Fatigue: Staff worry about job security. Reframe automation as “digital coworker,” not replacement, and offer upskilling.
- Scope Creep: Start with a narrow task. Success breeds enthusiasm, but expanding too fast can overwhelm governance.
- Ongoing Tuning: Treat the agent like a new hire—it needs reviews, feedback, and periodic retraining.
Address these early to protect your Automation ROI and sustain trust.
A Four-Step Plan to Get Started
1. Map the Pain Points
Run a one‑day workshop. List admin tasks, time spent, and error rates. Rank by impact and feasibility.
2. Choose a Pilot
Select one workflow with clear metrics (e.g., eligibility checks). Define success: minutes saved, dollars gained.
3. Deploy and Measure
Integrate the agent in a sandbox, train staff, go live, and track KPIs weekly for 8–12 weeks.
4. Scale and Govern
If goals are met, move to the next task. Form an “AI stewardship committee” including clinical, IT, and compliance teams to oversee expansions.
Following this phased path keeps risk low while unlocking compounding Automation ROI over time.
Conclusion
Paperwork should never stand between a patient and care. Agentic AI removes that barrier by performing the invisible chores that clog community health workflows. The result is simple: more time with patients, healthier bottom lines, and happier teams. Real clinics have already proven the gains, and the entry cost is lower than many expect. If you want to see higher Automation ROI next quarter—measured in both dollars and healthier neighbors—now is the time to pilot your first agent.








