
Key Takeaways
- Without connected systems, physicians miss key history, causing delays, errors, and repeat work that harms care quality.
- AI uses probabilistic matching across names, dates, diagnoses, and clinical patterns to unify patient identities and histories.
- They oversee strategy, tool selection, rollout, training, and data governance to enable seamless, compliant EMR integration.
- Doctors access complete, real-time patient views, enabling proactive care, fewer errors, and personalized treatment plans.
- As AI evolves, it will enable early interventions and real-time alerts, empowering patients to manage their entire health journey.
Imagine visiting a new doctor—perhaps a specialist or one you’ve moved to a new city to see. You sit down, ready to explain your entire medical history from scratch: past illnesses, medications, allergies, surgeries, and even that obscure family condition. Now, imagine if, before you even opened your mouth, your new doctor had a complete, accurate, and up-to-date picture of your health journey, seamlessly pulled from every hospital, clinic, and lab you’ve ever visited.
This isn’t a futuristic dream; it’s the promise of “smart technology”—what many are calling Artificial Intelligence (AI)—when applied to healthcare. For too long, our medical information has been scattered across various digital filing systems, commonly referred to in the healthcare world as Electronic Medical Record (EMR) systems. These separate systems, often from different providers or even different departments within the same hospital, create a fragmented view of your health, leading to inefficiencies, potential errors, and considerable frustration for both patients and healthcare professionals.
However, a dedicated effort is now underway to bring these pieces together. This effort is often guided by an “Automation Center of Excellence” (Automation CoE), a specialized team within healthcare organizations that focuses on making processes more intelligent and more connected. They are the architects of this quiet revolution, ensuring that the incredible power of technology is used to build a more unified and effective healthcare system.
Also read: The Role of a HyperAutomation CoE in Standardizing Automation-as-a-Service Across Enterprises
The Challenge: Why Patient Data Gets Stuck
To truly appreciate the solution, we must first understand the problem. Think of each hospital, clinic, or even a small doctor’s office as having its unique digital ledger for patient information. These ledgers, or EMR systems, are like different brands of software, each speaking its digital language and storing data in its particular way.
Now, imagine trying to combine recipe cards from ten different kitchens. Each kitchen has a unique writing style, uses different measurements (some use cups, while others use grams), and even has different names for the same ingredients. Trying to create one comprehensive cookbook from these disparate sources would be a nightmare. This is precisely the challenge healthcare faces with fragmented patient data.
The consequences of this scattered information are far-reaching and often profound:
- Incomplete Picture for Doctors: A physician treating you might not have access to crucial details about your past treatments, medications prescribed by another specialist, or even a previously diagnosed allergy. This “missing piece” can lead to repeated tests, delayed diagnoses, or, in critical situations, potentially harmful medical decisions.
- Patient Frustration and Repetition: How many times have you filled out the same lengthy medical history forms at different doctor’s offices? Or did you have to explain your chronic condition repeatedly to every new specialist? This isn’t just annoying; it’s a drain on your time and energy when you’re already feeling unwell.
- Increased Risk of Errors: When information isn’t readily available, the chances of medical errors, such as prescribing a medication that interacts negatively with another medication you’re taking or overlooking a critical health warning, increase significantly.
- Inefficient Healthcare Delivery: Healthcare professionals spend valuable time hunting for information, calling other offices, or deciphering incomplete records. This takes away from the time they could be spending directly caring for patients.
- Hindrance to Public Health: Understanding disease patterns, tracking outbreaks, and improving public health strategies relies on comprehensive data. When patient information is siloed, it becomes challenging to obtain a thorough and accurate picture of community health trends.
These “digital islands” of patient data make it incredibly hard to provide truly coordinated and continuous care.
The Solution: How Smart Technology Connects the Dots
This is where “smart technology” steps in, acting like a highly sophisticated digital detective, tirelessly working to connect the scattered pieces of your medical story. We’re discussing technologies such as Artificial Intelligence (AI) and Machine Learning (ML). Don’t worry about the complex technical terms; think of it simply as computer programs that are incredibly good at recognizing patterns and learning from experience.
Here’s how this “smart technology” helps bridge the gaps between different healthcare records:
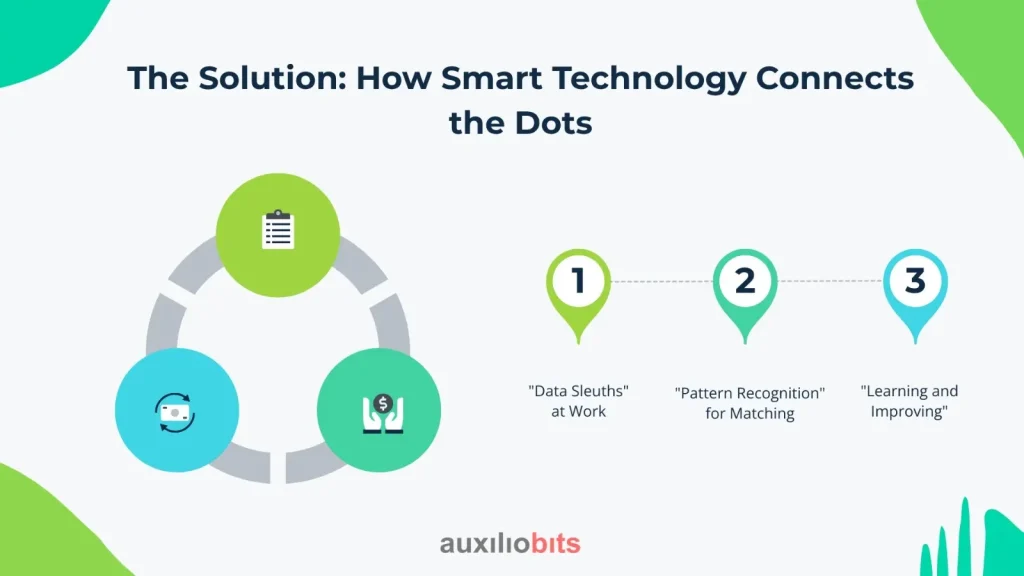
- “Data Sleuths” at Work: Imagine AI algorithms as super-detectives. They are designed to sift through enormous amounts of patient data from various sources – different EMR systems, lab results, imaging reports, and even notes from doctors. Unlike human detectives, they can process millions of pieces of information in mere seconds.
- “Pattern Recognition” for Matching: The core of this technology lies in its ability to find connections. It looks for commonalities that indicate records belong to the same person. This isn’t just about matching names and birthdates, which can be tricky due to typos or common names. AI goes deeper, examining a combination of factors, including addresses, phone numbers, past diagnoses, medication histories, and even subtle patterns in clinical notes. For example, if “John Smith” from one clinic has a birthdate of “January 1, 1970” and a diagnosis of “Type 2 Diabetes,” and another record for “Jonathan Smyth” from a different hospital has a birthdate of “January 1, 1970”. Additionally, it shows a history of “diabetes management,” and the AI can intelligently suggest that these are likely the same individual, despite the slight name difference. It uses complex probability to determine the likelihood of a match, far surpassing what manual review could achieve.
- “Learning and Improving”: This is the “smart” part of innovative technology. The more data it processes and the more human healthcare professionals confirm or correct its findings, the more accurate it becomes at making accurate assessments. It learns from its “mistakes” and refines its understanding of what constitutes a proper patient match. This continuous learning process means the system becomes increasingly precise and reliable over time.
The benefits of this data connection are transformative for patient care:
- A Complete Patient View: Doctors gain a holistic, 360-degree understanding of your health journey. They can see your complete medical history, allergies, all medications you’ve ever been prescribed, and every test result, no matter where they were performed. This complete picture empowers them to make more informed and effective decisions.
- Safer Healthcare: With comprehensive data at their fingertips, healthcare providers can drastically reduce the risk of medication errors, avoid redundant tests, and ensure treatments are tailored to your specific needs and past medical history.
- More Efficient Operations: Less time is wasted on administrative tasks, such as searching for records or repeatedly entering patient information. This frees up healthcare staff to focus on what truly matters: providing direct patient care.
- Personalized Treatment Plans: When a doctor has your complete health story, they can create truly customized treatment plans, taking into account your unique predispositions, past responses to treatments, and overall health trajectory.
- Empowering Research and Public Health: Unified data provide a rich resource for medical research, helping scientists identify new trends, better understand diseases, and develop more effective treatments. It also allows public health agencies to track diseases, monitor population health, and respond more effectively to health crises.
The Power Behind the Progress: The Automation CoE
Making this “smart technology” work seamlessly within the complex world of healthcare isn’t something that happens by accident. It requires a dedicated, strategic approach. This is where the Automation Center of Excellence (Automation CoE) plays a crucial, often unsung, role.
Think of an Automation CoE as the specialized command center within a hospital system or healthcare organization that is solely focused on making things run smarter and more efficiently using technology. They are the experts who understand both the potential of advanced tools, such as AI, and the unique needs and challenges of healthcare.
Their responsibilities are vital to the success of patient data matching:
- Setting the Vision and Strategy: The CoE doesn’t just implement technology; it defines why and how automation, including AI for data matching, will benefit the organization and, most importantly, the patients. They create a roadmap that outlines the problems the technology will solve and the desired outcomes.
- Choosing the Right “Smart Tools”: Just like a chef selects the right ingredients for a recipe, the Automation CoE carefully evaluates and chooses the most suitable AI and other innovative technologies for patient data matching. They ensure these tools are robust, scalable, and capable of handling the sensitive nature of health information.
- Implementation and Oversight: They are responsible for the nitty-gritty of getting these systems up and running. This involves working with IT teams, integrating new tools with existing EMR systems (a significant challenge!), and ensuring everything functions smoothly. They also continuously monitor the performance of these automated systems, making adjustments as needed.
- Training and Adoption: Introducing new technology can be daunting. The CoE plays a critical role in educating healthcare professionals – doctors, nurses, administrative staff – on how to use these new tools effectively. They ensure that everyone understands the benefits and feels comfortable integrating them into their daily work.
- Ensuring Security and Privacy: Paramount Concern: This is arguably one of the most crucial aspects of their role. Patient data is incredibly sensitive. The Automation CoE is responsible for implementing stringent security protocols and ensuring that all data matching and sharing comply with strict privacy regulations (like HIPAA in the United States). They build safeguards to prevent unauthorized access and ensure that patient information is always protected, even as it is being connected and shared, to improve care. They understand that trust is fundamental in healthcare, and robust security is key to maintaining that trust.
- Standardization and Best Practices: As they roll out these solutions, the CoE works to standardize processes and establish “best practices” across different departments or even different facilities within a healthcare network. This ensures consistency and reliability in data matching.
In essence, the Automation CoE brings expertise, strategic thinking, and meticulous attention to detail to a complex challenge. Without a dedicated team guiding these efforts, the promise of connected patient data would remain just that – a promise. They ensure a systematic, secure, and ultimately, patient-centric approach to integrating valuable health information
Real-World Impact and the Future
Let’s think about what this looks like in practice. Imagine a patient, Sarah, who arrives in the emergency room after an accident. In the past, the ER doctor might have had to rely on Sarah’s memory or scramble to call her primary care physician for her medical history. But with innovative technology connecting her data, the ER doctor immediately sees that Sarah has a severe penicillin allergy, a pre-existing heart condition, and is currently taking specific blood thinners. This instant access to crucial information enables rapid, life-saving decisions, thereby avoiding potential complications.
Or consider John, who has a rare chronic illness and sees multiple specialists across different hospitals. In a fragmented system, each specialist might only see a piece of John’s health puzzle, leading to disjointed care. But with connected data, every specialist has access to all of John’s test results, treatment plans from other doctors, and medication adjustments, ensuring truly coordinated and comprehensive care for his complex condition.
The future of healthcare, empowered by this intelligent data matching, is even more exciting:
- Even More Seamless Data Exchange: The goal is to make data flow between different systems as effortlessly as water. This means less friction, faster access, and a more comprehensive picture of patient health.
- Predictive Health Insights: Connected data, analyzed by innovative technology, can begin to identify patterns that predict potential health risks even before symptoms appear. This could lead to earlier interventions, preventative care strategies, and better long-term health outcomes for individuals and communities.
- Empowering Patients: Imagine a future where you, as a patient, have a secure, easy-to-understand portal that consolidates all your medical information in one place, regardless of where you received care. This empowers you to be a more active participant in your health journey.
Conclusion
The journey to truly connected patient data is a significant undertaking, but the benefits for patients and the healthcare system as a whole are immeasurable. Fragmented records have been a silent hurdle in providing the best possible care for too long. However, with the strategic application of “smart technology”—what we call AI —guided by the dedicated efforts of an Automation Center of Excellence, we are moving towards a future where every piece of your health story is readily available to those who need it, when they need it.
This shift isn’t just about efficiency; it’s about transforming healthcare into a more precise, personalized, and proactive system. It’s about ensuring that every patient receives safer, more informed, and ultimately, better care. Imagine a future where your entire health story is always available to those who need it, whenever they need it, enabling the best possible care. That future is not just possible; it’s being built, one connected record at a time.








