
Key Takeaways.
- Agents, not scripts—Autonomous agents backed by MCP perceive, reason, act, and learn, forming self-healing workflows.
- Regulation is the spur—The 2026 CMS deadline leaves no room for manual handoffs.
- ROI is proven—Early adopters cut adjudication times by eighty-four percent and saved thousands of labor hours.
- Security is built-in—zero-trust enclaves and compulsory human review processes keep payers aligned with HIPAA and state laws.
- The future is parametric—Streaming biosensor data will trigger live premium tweaks, and MCP agents are the only practical way to scale the math.
A mid-sized U.S. health plan now manages nearly two billion claim lines each year. Every submission hops between clearing‑house scrubbers, EDI gateways, mainframes, and at least one manual phone call. A missing date of service or a mismatched CPT code can bounce the file back to the provider, triggering recursive appeal cycles that drain goodwill on both sides. The administrative weight—approximately a quarter of a trillion dollars a year—accounts for almost one-third of total premium revenue.
In January 2024, the Centers for Medicare & Medicaid Services finalized the “Interoperability and Prior Authorization” rule, which compresses decision windows and requires payers to publish denial metrics. The clock is ticking: missed deadlines after January 1, 2026, can result in fines, interest, or even loss of star ratings in Medicare Advantage. Boards are therefore asking a simple question: can software do the clerical work faster and more fairly than our current mix of cubicles and macros? The answer turns out to be yes, provided the software behaves autonomously, cooperates through an open protocol, and provides explanations for its reasoning.
Also read: Ethical Considerations When Deploying Autonomous Agents.
The Claims Pain Points
Before prescribing a cure, we must diagnose the recurring aches:
- Glacial prior authorization—The median turnaround is ten days; yet, as of 2026, CMS will mandate a seven-day standard and a seventy-two-hour urgent decision.
- Data fragments, such as ANSI 837, HL7 v2, FHIR R5, flat PDF attachments, and even handwritten faxes, are all mixed in the same queue.
- Opaque denials—Providers often receive one-line denial codes with no clinical narrative, fueling costly appeals.
- Manual rework loops— Every policy tweak breaks fragile RPA macros, pushing staff back to spreadsheets.
- Fraud leakage—Slow investigations allow bad actors to siphon an estimated ten percent of payouts.
Hidden inside these buckets are dozens of micro-frictions: portals that log out after ten minutes. These claims must be faxed because a downstream system refuses modern PDF/A and coverage tables that differ by a single punctuation mark. Entire cottage industries of billing clerks spend their days chasing status updates instead of patient care.
What Makes an Agent “Autonomous”?
An autonomous agent is more than a scripted bot; it combines four native skills:
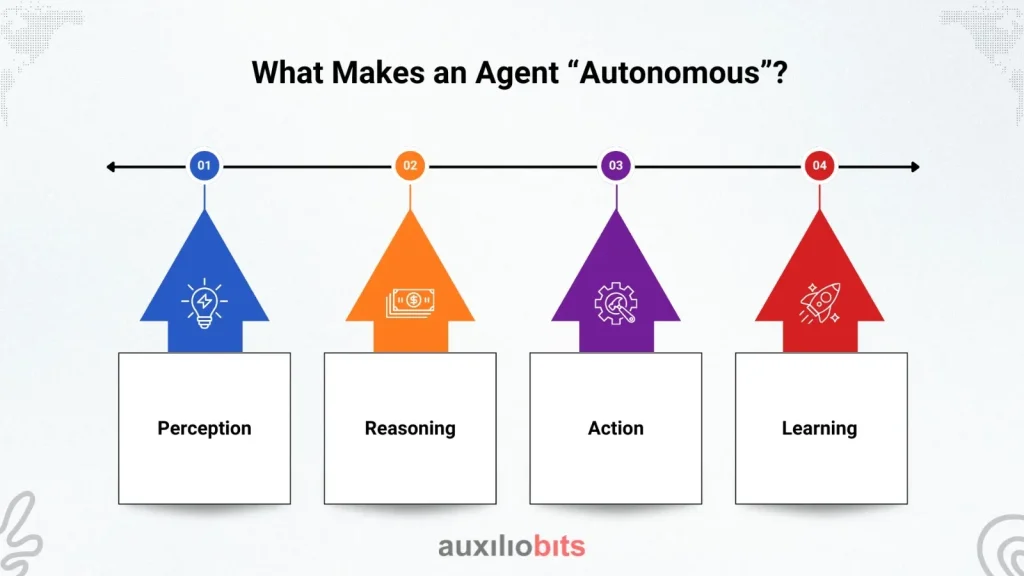
- Perception—Parses structured records and free text via APIs, OCR, or speech recognition.
- Reasoning—Selects next steps using policy graphs, chain-of-thought LLM prompts, or reinforcement learning.
- Action—Invokes APIs, writes ledger entries, or escalates to human teammates.
- Learning—Captures results and refines its tactics without manual re‑coding.
Each agent publishes a capability manifest (what it can do), a context contract (what data it needs and emits), and a goal schema (what outcome defines success). MCP Protocol serializes the trio into signed packets, allowing agents to be assembled like Lego bricks while still honoring HIPAA boundaries. Think of an agent as a tireless colleague with perfect recall and a KPI-aligned compass.
MCP Protocol—The Nervous System of Multimodal Claims Automation
Why MCP?
Point-to-point integrations are brittle and expensive to certify. MCP offers a stateless envelope with three primitives—Memory, Compute, and Plan—so any agent can ask for help without hard-coding function calls. Memory objects hold encrypted PHI, Compute objects describe tool invocations, and Plan objects reveal the task graph. The reference implementation is under 300 lines, allowing corporate security teams to audit every byte of code.
Because MCP is stateless, a rules engine can be swapped for a tuned Llama-3 model overnight, and the rest of the mesh continues to operate smoothly. Traditional service-bus orchestration relies on schemas and long certification cycles. Any alteration ripples through dozens of WSDLs, freezing innovation. MCP flips the model: each packet carries its schema, allowing agents to negotiate contracts at runtime and decouple release cadences. Future compliance tweaks—such as quantum-safe encryption or new EU residency laws—become schema upgrades rather than system rewrites.
Claims‑Specific Mapping
| MCP Primitive | Claims Usage | Example Agent |
| Memory | Eligibility history, benefit ledger, provider contracts, prior-auth outcomes | Memory Agent |
| Compute | FHIR lookups, actuarial risk models, and NLP on clinical notes | Compute Agent |
| Plan | Intake → eligibility → risk → adjudication → payment | Planner Agent |
A Walk Through the Agentic Claim Journey
Explore how autonomous AI agents collaborate across the health insurance claims lifecycle—intelligently validating, verifying, approving, and explaining every step.
- The Intake Gatekeeper Agent validates the EDI envelope, extracts key fields, and attaches vector embeddings for context retrieval.
- Eligibility Agent queries clearinghouses and real-time FHIR endpoints; if coverage is unclear, it generates a SMART-on-FHIR questionnaire to clarify the situation.
- The Prior-Author Conductor consults clinical guidelines and CMS timers, issuing instant approvals for low-risk procedures.
- The Fraud Sentinel Agent runs graph analytics on provider networks and flags anomalies for human review only when the risk exceeds a threshold.
- The Adjudication Agent applies contract math, bundled payment rules, and carve-outs to determine the allowed amount.
- The EOB Narrator Agent drafts a plain-language Explanation of Benefits in English and Spanish, citing policy passages.
- The feedback Loop stores outcomes in vector memory, allowing future decisions to learn from past appeals.
Each hop emits an audit event, creating a live topology map that risks officers and providers can monitor in real-time, reducing “where is my money?” phone calls.
Under the Hood—Reference Architecture & Tech Stack
Delve into the technical backbone powering agentic claims—from secure data layers and real-time events to scalable LLM runtimes and policy-aware orchestration.
- Data layer—Delta Lake for finance facts; FHIR R5 store for clinical context; immutable WORM buckets for audits.
- Event fabric—Kafka carries MCP envelopes; a schema registry enforces PHI tagging; every message is signed with short-lived JWTs.
- Agent runtime—Orchestrators like CrewAI spawn containerized agents, each with its own GPU or CPU slice.
- LLM choice—Domain-tuned Llama-3-70B hosted in confidential-compute enclaves so prompts stay shielded.
- Policy engine—Open Policy Agent captures CMS rules and state mandates in Rego.
- Synthetic data—Diffusion techniques generate fake yet statistically realistic claims for stress tests.
A reference deployment runs on Kubernetes with GPU pools that auto-scale during evening provider batches. Observability is achieved through OpenTelemetry streams, which are integrated into Datadog, enabling the correlation of latency spikes with sandbox model updates.
Quantifying Impact—Pilot Results 2024–2025
| Metric | Pre-Agent | Post-Agent |
| Average adjudication time | 12.5 days | 1.9 days |
| Employee hours saved | — | 15 000 per month |
| Operational cost index | 1.00 | 0.65 |
| Denial reversal rate | 17 % | 8 % |
| Prior-auth SLA breaches | 23 % | 5 % |
Most payers saw cash payback within nine months. Beyond raw speed, pilots uncovered surprising second-order benefits. Provider satisfaction scores jumped because portal dashboards now show real-time claim status instead of cryptic batch updates. Members saw fewer surprise bills because eligibility misfires plummeted. Finance teams gained a new weapon against reserve volatility: continuous adjudication generates smoother IBNR curves and tighter accruals.
Even medical management benefited—fraudulent billing patterns surfaced earlier, allowing special investigation units to intervene before the payout cleared, not months later. These softer gains rarely appear in the first ROI slide, yet executives consistently rate them as game-changers.
Security, Compliance, and Ethical Guardrails
- Zero-trust segmentation—Every claim lives in a just-in-time enclave; agents can access only declared fields.
- Immutable provenance—Each MCP hash lands in a private Ethereum sidechain, creating non-repudiable logs.
- Human review of denials—Planner Agents route any adverse decision to a licensed clinician, meeting CMS orders.
- Differential-privacy dashboards— Added noise stops patient re-identification while keeping population stats functional.
- Encrypted prompt vault—LLM prompts and outputs are redacted and sealed for retrospective audits.
Robust governance does not end with encryption. Every agent carries a provenance stamp that includes Git commit hash, model checksum, and configuration fingerprint. When an audit occurs, compliance officers can replay the exact version of code and policy in force at the time of the decision—a feature that is almost impossible with legacy RPA, where scripts drift quietly on individual desktops. Ethical oversight boards appreciate that MCP packets expose the agent’s declared goal and chosen plan; if a behavior deviates, sentinel monitors raise an alert. Combined, these measures turn the agent mesh from a perceived risk into a verifiable control surface.
Implementation Road Map—Four Levels of Maturity
| Level | Scope | Typical Timeline |
| L1—Task Bots | OCR and RPA keystrokes | 3 months |
| L2—Single Agent | Eligibility verification | 6 months |
| L3—MCP Mesh | End-to-end adjudication | 9–12 months |
| L4—Real-time pricing | Wearable data, dynamic premiums | 18 months |
Quick wins emerge at L2, where one Eligibility Agent eliminates the most common rejection reason—coverage lapse. Forward-leaning payers create cross-functional “agent guilds” so that nurses, adjusters, data scientists, and lawyers co-design each upgrade, thereby trimming resistance.
Moving between maturity levels is not purely a tech exercise. CFOs must revisit cost-allocation models, legal teams must revise EDI trading-partner agreements, and HR needs new job ladders for staff transitioning from data entry to bot supervision. Change management also encompasses front-line call centers, where dashboards now display live agent progress, enabling representatives to respond to member queries without requiring escalations to higher levels.
Successful programs charter a cross-functional steering committee and publish bi-weekly burn-down charts tracking defects fixed, SLA hits, unfinished stories, and production savings. That transparency calms skeptics, keeps budget gates, and turns stakeholders into evangelists.
Challenges and Mitigations
Learn how agentic systems confront real-world risks—handling model drift, prompt threats, data standard clashes, and edge cases with precision and resilience.
- Model drift—Quarterly CPT updates can break predictions; nightly fine-tunes keep Compute Agents current.
- Prompt injection—Free-text EHR notes might hide malicious code; a sanitation agent strips unsafe tokens.
- Standards fragmentation—EDI, HL7, and FHIR collide; Memory Agents translate to a canonical schema.
- Edge-case explosion—Rare newborn coverage plus secondary payer scenarios; a Safeguard Agent routes novelties to senior reviewers.
Future Outlook—Parametric Cover and Real‑Time Pricing
Wearable streams already deliver heart rhythm and glucose curves. By 2030, those metrics will reside in MCP Memory shards. Planner Agents will adjust premiums every week, much like usage-based auto insurance. Picture a continuous glucose monitor predicting a crash: an agent could pre-authorize an ER visit before the ambulance arrives, saving minutes and money. Regulators will likely cap frequency and require opt-in, but the shift toward live, context-aware coverage is irreversible.
Conclusion
Autonomous agents orchestrated through the MCP Protocol are turning claim lines into living digital supply chains. Payers that act today will trim waste, satisfy regulators, and reimburse care faster—freeing patients and providers to focus on healing rather than paperwork.Autonomous agents orchestrated through the MCP Protocol are turning claim lines into living digital supply chains. Payers that act today will trim waste, satisfy regulators, and reimburse care faster—freeing patients and providers to focus on healing rather than paperwork.








