Key Takeaways
- Automation streamlines healthcare revenue cycle management by reducing manual errors, accelerating claims processing, and enhancing patient registration, ultimately leading to faster reimbursements and more efficient financial workflows for providers.
- AI-powered coding and robotic process automation cut claim denials and accelerate billing cycles, allowing healthcare organizations to enhance cash flow while maintaining compliance with constantly evolving regulations.
- Automated eligibility verification and patient self-service tools simplify front-desk workflows, improve data accuracy, and enhance the patient experience by reducing wait times and providing transparent billing.
- Real-time dashboards and advanced analytics enable healthcare providers to monitor key financial metrics like denial rates and collections, facilitating proactive decisions that boost revenue and operational efficiency.
- The future of RCM automation will leverage AI, ML, blockchain, and interoperability to create more predictive, secure, and seamless workflows, driving sustainable financial health and patient trust in value-based care models.
Revenue cycle management has always been a challenging, if not unpleasant, part of healthcare. Many organizations still rely on cumbersome, labor-intensive manual processes. A coding error or typo in a patient’s information can delay claims or result in denials, ultimately costing providers time and money. In the real world, unfortunately, estimates suggest that up to 20% of original claims are denied due to minor errors.
Regulatory complexity is part of the burden. Changing payer needs and healthcare regulations continually evolve, which can slow down staff and lead to an administrative burden, resulting in delayed reimbursement. To make matters worse, patients are now expecting faster and more transparent billing practices, something manual systems are incapable of delivering.
How is Automation Revolutionizing RCM?
Revenue cycle management is being revolutionized through automation, leveraging powerful technologies such as artificial intelligence (AI), machine learning (ML), and robotic process automation (RPA). These technologies automate front-desk activities through back-end billing.
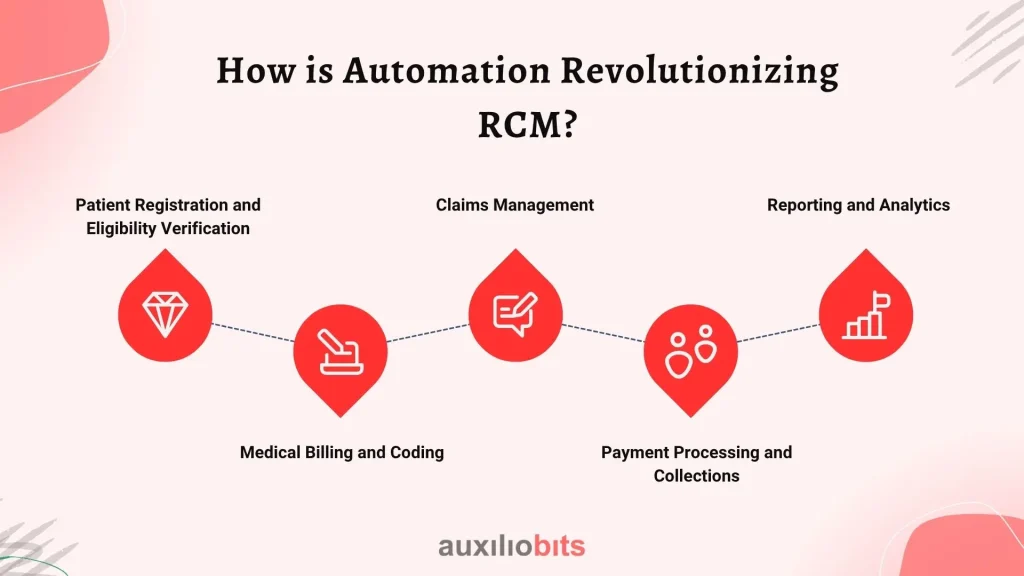
1. Patient Registration and Eligibility Verification
Eliminate the clipboard and endless forms. Automated applications verify insurance coverage in seconds by connecting directly to payer systems. AI-based chatbots and e-intake forms also enable patients to fill out their data, reducing errors and streamlining the process.
2. Medical Billing and Coding
AI software can process clinical documentation and code using precise medical codes without human intervention. This reduces expensive coding errors and accelerates billing, allowing claims to be sent accurately the first time.
3. Claims Management
With RPA, claims are monitored in real time. If an error occurs, the system flags it before submission. When a claim is rejected, automation can readily identify the mistake, correct it, and resubmit, drastically minimizing turnaround time and enhancing cash flow.
4. Payment Processing and Collections
Payment Processing and Collections from Patients Automated payment products offer patients several easy ways to make payments through text links, websites, or mobile applications. AI can even predict which patients are likely to struggle with payment and offer them special payment plans in advance, thereby improving overall collection rates.
5. Reporting and Analytics
Data is likely one of the most significant game-changers. Automation provides real-time dashboards that display denial rates, collection efficiency, days accounts receivable (D/A/R), and other key metrics. With this information, practices can identify problems early on and make wiser financial decisions.
Benefits of RCM Automation
Automation in revenue cycle management delivers transformative advantages that streamline operations and improve financial outcomes for healthcare providers. Below are some of the key benefits:
- Improved Efficiency: Employees get to work on patients, not paperwork.
- Fewer Errors: AI reduces coding and billing errors.
- Enhanced Patient Experience: Faster, more transparent billing builds trust.
- Cost Savings: Reduced manual labor implies lower administrative costs.
- Improved Compliance: Computerized systems are current with ever-evolving laws.
Real-World Impact
Automation is not theory; it’s delivering real results. One hospital reduced its claim denial rate by 15% in six months using AI-based coding software. Another clinic reduced registration errors by 30% using automated eligibility verification. These are not exceptions; they are a sign of the direction the industry is taking.
The Future of RCM Automation
In the future, look for even more intelligent automation. AI and ML will become increasingly proficient at predicting denials and suggesting corrections before claims are even submitted. Blockchain will bring new levels of security and transparency. And better interoperability will allow systems to “talk” more simply to each other across the entire healthcare system. As value-based care models become increasingly popular, real-time financial analytics will become a prerequisite, making sophisticated RCM automation a nice-to-have, rather than a must-have.
Conclusion
The switch to automated revenue cycle management is more than just a technological upgrade; it’s a strategic approach to achieving long-term financial success, enhancing the patient experience. By clearing bottlenecks, reducing errors, and empowering patients, healthcare organizations can thrive in a changing environment. Ready to future-proof your revenue cycle? Start learning more about automation tools today and provide your practice with the competitive edge it needs in tomorrow’s healthcare economy.