The COVID-19 pandemic has driven several manual processes to automated modes of functioning. Automation has made inroads in almost all sectors including healthcare. Healthcare professionals have understood the significance of emerging technologies such as RPA, AI, ML, Cloud, Big Data, etc., and their positive impact on streamlining various processes and workflows.
Healthcare services include several repetitive administrative and non-administrative processes that can be easily automated. One such process is claims management!
- Claim processing in healthcare is a tedious and time-consuming process that involves several stakeholders.
- Claims processing goes through several manual processes that are prone to errors and cause delays.
- RPA bots streamline claims processing by automating all rule-based manual tasks to enhance efficiency and speed.
- Technologies like AI, ML, IoT, Big Data, and the Cloud augment RPA for better data management and collaboration of stakeholders.
What is Claims Management in Healthcare?
Claims processing is a long-drawn process that starts when a patient has an appointment with the doctor till the time bill is paid. It is a complex process that involves several stakeholders and detailed documentation. Relevant data needs to go through numerous steps until the payment is completed.
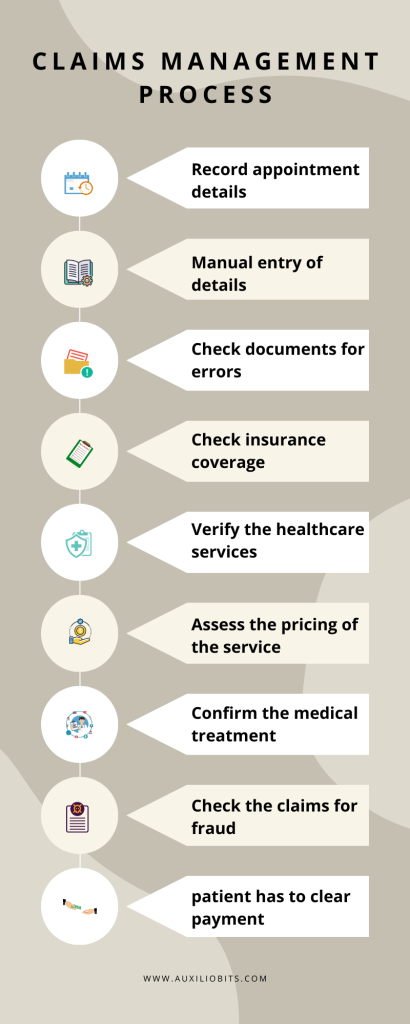
A typical claims management process goes through the following steps:
Step 1: When a patient meets a doctor, the details of the appointment and services provided are recorded on paper or via email.
Step 2: The paper claims are manually entered or scanned.
Step 3: The documents are checked for errors and duplicity.
Step 4: Checks are conducted to find out if the patient had insurance coverage at the time when the service was provided.
Step 5: Further checks are conducted to confirm if the doctor or healthcare facilities used are covered in the insurance plan.
Step 6: The pricing of the service is analyzed to ascertain the amount that will be covered by insurance and if the patient is required to pay any amount.
Step 7: Various checks such as what is included in the patient’s insurance coverage, whether the services used are medically necessary, and more.
Step 8: The insurance claims are verified to ensure that they are not fraudulent.
Step 9: After all checks and verifications, the doctor is paid and the patient is sent an Explanation of Benefits that provides details of the medical expenses that were covered and that were not. It gives the patient an indication of the amount he is expected to pay.
Step 10: The patient has to clear the billed amount.
As can be seen, the entire claims management function involves several manual processes that are tedious and time-consuming. These processes are vulnerable to human errors at different stages impacting the overall outcome. Any undetected error can cause high losses. Delays at any stage can slow down the process providing a poor patient experience.
Claims processing entails the collaboration of several stakeholders such as the patient, insurance company, healthcare administrative and non-administrative staff, etc. Effective collaboration is a problem area in traditional systems. Lack of effective collaboration causes delays and other issues in processing claims.
Besides these, manual claims processing also faces problems like managing variations in medical insurance policies offered by different companies, and other aspects of insurance claims. This is because there is no standardized format for the insurance coverage offered by different private and public sector companies. For instance, some insurance providers may accept insurance forms through web portals while others may need them via email. Such variations are difficult to manage.
In manual systems customizing the claims process according to the specific needs of a patient is almost impossible.
Most healthcare service providers need to process large volumes of claims each day which requires dedicated time and effort from employees. Processing such large volumes of claims manually can generate backlogs and impact the timely care of patients. It can also create a backlog of payments to medical service providers.
Healthcare claims processing involves the management of large volumes of unstructured data which makes it difficult for the staff to manage.
Manual processing also requires a large number of skilled staff members to work in tandem.
The manual paper-based processes have been replaced by digital techniques such as processing electronic medical records, data management using spreadsheets, etc. However, there are some lacunae in these methods also. This is because although computers are used in these processes, it is humans who are performing activities such as data entry, data checking, etc. Hence, these methods are slow and error-prone.
This is where automation has a role to play!
The healthcare sector can leverage claim processing automation to streamline processes such as accounts payable, contract management, medical claims, patient onboarding, and more.
Automation bots streamline all processes related to claims management that includes simple data entry to complex claims processing.
Technologies such as Robotic Process Automation (RPA), Artificial Intelligence (AI), and Machine Learning (ML), are the chief automation technologies that are leveraged alongside technologies like Big Data, Cloud, Internet of Things (IoT).
How to Automate Claims Processing?
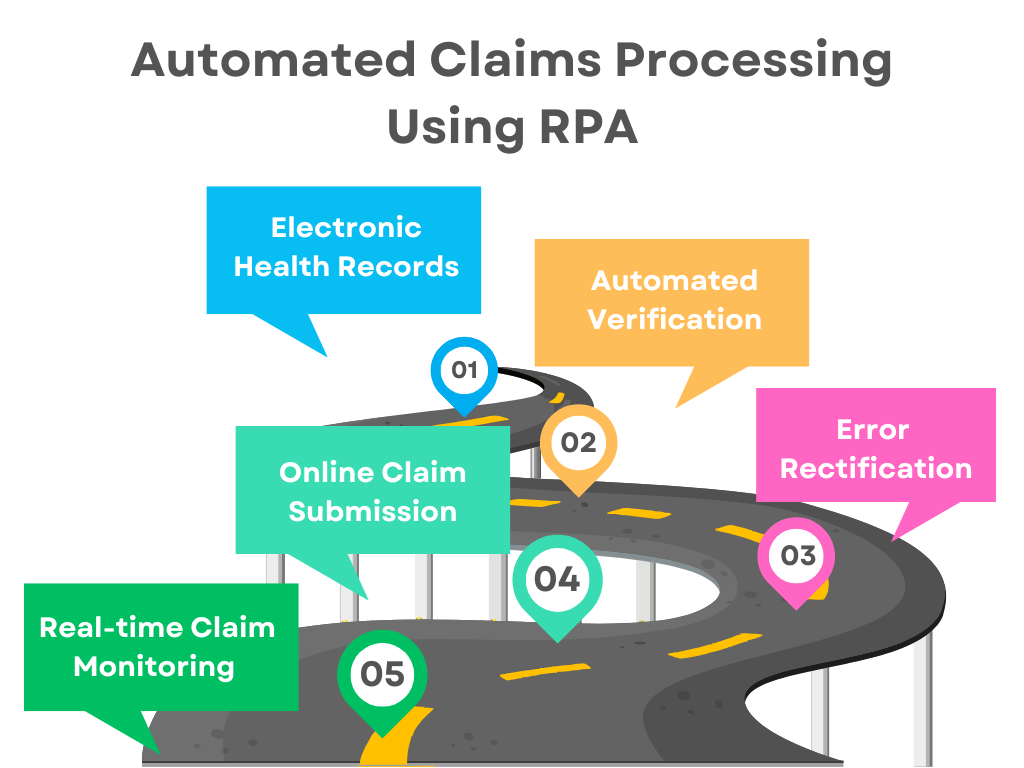
1. Use Electronic Health Records (EHRs)
The first step for automating claims processing is to replace paper-based medical records with EHRs. EHRs simplify data management. They provide easy access to patient’s treatment data in the claims management system. Besides, EHRs facilitate an interoperable platform for medical claim processing. They provide transparency in the claims management process thereby enhancing the patient experience.
2. Automate Verification
An insurance claim passes through a series of tests to authenticate the claim. These checks include verification of the eligibility of the claim, whether the patient is entitled to the claim, if the claim is fraudulent, etc. All these verifications can be automated using Robotic Process Automation (RPA). RPA bots perform these checks accurately and at a fast speed.
3. Rectify Errors
Errors in claims processing can lead to denials. In some cases, these errors can prove to be very costly resulting in losses. Hence, errors must be identified well in time and corrected. RPA bots can easily detect errors quickly thereby avoiding delays in the process. Artificial Intelligence-based bots offer suggestions to rectify these errors.
4. Online Claim Submission
Online claim submission simplifies the process. Patients can submit the form online. Insurance companies, patients, healthcare representatives, etc. can easily access information through a centralized repository. They can incorporate any changes required. Online claims also minimize paperwork. A cloud-based claims processing environment makes it easier for various stakeholders to track payments.
5. Real-time Claim Monitoring
Wearable devices such as fit bits have become extremely popular. These devices facilitate real-time monitoring of various parameters. Doctors can provide the proper treatment for various health conditions online. The availability of medical records and treatment details facilitates hassle-free claims processing in real time.
Some of the Technologies Deployed for Claims Processing Include:
Robotic Process Automation:
RPA bots automate several rule-based processes such as data entry, validation of data, etc. RPA eliminates human errors and speeds up the process.
Big Data:
Large volumes of data are processed in claims management. Big data streamlines data management.
Cloud:
Cloud technology is leveraged to facilitate data handling multiple sources. The cloud helps in seamless collaboration between various stakeholders thereby enhancing the efficacy of the process.
Internet of Things (IoT):
IoT devices have found extensive application in the healthcare sector. IoT-based wearables facilitate real-time monitoring of patient data. They help in speeding up the claims management process.
Artificial Intelligence:
Artificial Intelligence is leveraged to make claims management automation intelligent. AI gathers data, analyzes it, and provides valuable insights that streamline claims processing.
If you are looking to enhance the efficiency of claims management in your services, connect with the experts at Auxiliobits!
Our professionals have years of experience in providing automation software to healthcare service providers across the globe.
The in-depth technical knowledge of our professionals helps us offer the best automation solution for your services.
Our professionals are not only experts in the technical domain but are knowledgeable about the functioning of the claims management process in the healthcare sector.
We provide cost-effective automation solutions that are industry-specific and domain-specific.
We offer after-sales support to ensure that the software works seamlessly.
We integrate the automation software with your existing systems with minimal disruption.
Call Us Now for Intelligent Automation for Claims Management!
Watch this space for more on automation solutions offered by Auxiliobits!




 April 15, 2024
April 15, 2024