
Key Takeaways
- Credentialing automation is an operational transformation, not just a software rollout. Success depends on clean baseline data, standardized workflows, and staff adaptability—not just system configuration.
- ModMed’s credentialing features streamline compliance through integration and context-aware validation. The ability to tie privileges directly to scheduling and documentation workflows eliminates costly errors and delays.
- Interoperability remains both a strength and a challenge. While ModMed integrates with core scheduling and reporting modules, limitations in external APIs and inconsistent state data still require human oversight.
- Automation delivers measurable value beyond administrative savings. Reduced compliance risks, fewer billing and scheduling errors, and improved patient continuity often outweigh the initial implementation costs.
- The next leap lies in intelligent, predictive credentialing. With AI-driven risk assessment and proactive monitoring, future systems could flag potential renewal delays or compliance gaps before they occur—turning credentialing into a preventive rather than reactive discipline.
Around 18% of the operational costs are consumed by administrative workflows for healthcare organizations. One of the most consistent pain points, and in this statistic lies a massive component—that’s credentialing and compliance. If you have ever needed to observe a medical staff office coordinator manage with spreadsheets, paper folders, and sticky notes while attempting to follow all the various licenses and hospital privileges, et al as they work towards being compliant, you know what I mean.
As a side note, we’ve come a long way with ModMed’s EHR in our attempts to meet these challenges, but as with any system, the learning curve and operational aspects will always be present. Having rolled out automation for credentialing in a variety of practice settings—from small dermatology clinics to multi-specialty groups—we’ve witnessed that realm and realized the opportunity that exists, as well as some frustrations that can arise when trying to digitize these manual processes.
Also read: Automating ModMed and eClinicalWorks Workflows with RPA
The Reality of Manual Credentialing
Most health system executives have war stories about credentialing nightmares. Think of this: Dr. Smith’s DEA license is expiring in two weeks, and the renewal application is at the bottom of someone’s in-tray, buried under a pile of papers. Meanwhile, the hospital’s credentialing committee meets only once a month—and missing that deadline is another two-month delay for renewal of those clinical privileges. Sound familiar?
Standardly, credentialing works are based on human memory and paper-based tracking systems, with reactive instead of proactive management. We have all worked in organizations where a person carries “the list” of dates inside their head or where important documents are kept in filing cabinets that only one person knows how to navigate.
This practice not only results in inefficiency—it creates actual danger. Expired certifications can be a patient care and onboarding nightmare, delaying a new provider’s first day of work by months and putting compliance issues on the line that regulatory bodies take very seriously. The Joint Commission won’t care that your credentialing coordinator was sick the week Dr. Jones’ board certification expired.
ModMed’s Approach to Credentialing Automation
Credentialing functionality built into their EMA (Electronic Medical Assistant) platform makes sense, and ModMed has it up to par. And rather than making staff move back and forth from system to system, credentialing data is part of provider profiles, scheduling, and documentation.
Credential tracking is centralized through digital provider files that include:
- Licensing information, including expiration tracking
- Board certifications and the recertification process
- Hospital affiliation and privileging paperwork
- Insurance network participations
- Continuing medical education credits
- Reports on background checks and drug screenings
There’s a difference, however. The integration layer within ModMed sets its credentialing off from standard tools. So by the time Dr. Martinez completes her procedure note in dermatology, the system already knows that she is presently privileged to perform procedures at the surgery center associated with our institution. That kind of immediate validation avoids the situation when providers mistakenly take a procedure out of their current privileging context.
However, the setup isn’t trivial. Delivering correct baseline data into the system is a bit of an upfront investment. We’ve seen practices spend weeks on data entry and importation of historical credentialing data, only to find that there are gaps or inconsistencies needing further verification. The old “garbage in, garbage out” principle comes into heavy play here.
Automated Alerts and Workflow Management
The alerting is one of ModMed’s best validation features. Instead of having to set your calendar to manually remind you, the platform will send you automated reminders at any intervals before the credentials expire.
Smart scheduling is especially useful with complicated renewal frequencies. And not all of those board certifications expire on a schedule that would be convenient: Some are 10-year cycles, while you need to check off annual maintenance of certification tasks in the rest. ModMed keeps track of these various timelines and may auto-initiate renewal procedures as necessary, considering that they need to allow for application processing times and meet with committee meetings to approve.
The automation goes beyond reminders—the workflow. When it’s time for him/her to renew his/her medical license, the platform can use automation to pull necessary forms, aggregate any supporting materials, and submit requests for approval to standard managers. This removes the common bottleneck of renewal processes getting hung up because no one knows whose desk the paperwork is currently sitting on.
(There’s a hitch—and here is where real-world implementation becomes interesting. Automated processes work only as well as the process they are based upon. Groups operating under fragmented credentialing processes realize that automation only magnifies already existing challenges instead of eliminating them. If your manual process today is five different people making their own ad hoc decisions, automating that chaos will not magically introduce consistency.
Integration Challenges and Considerations
ModMed’s credentialing module operates within a broader healthcare IT ecosystem, where smooth interoperability determines how efficiently providers can maintain compliance and privileges. While its integration capabilities offer practical advantages—especially around scheduling and reporting—they also expose a few structural limitations that healthcare organizations need to plan around.
Here’s a breakdown of the main integration insights and issues:
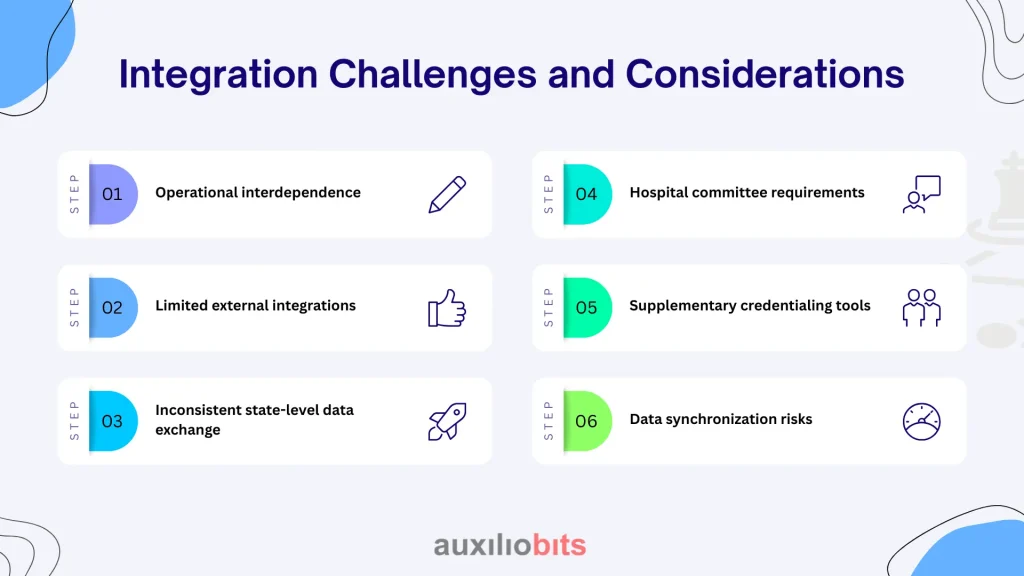
- Operational interdependence: The credentialing module ties closely with scheduling and reporting components. This helps prevent double-booking when providers await privilege renewals and ensures that network reports automatically exclude non-participating providers.
- Limited external integrations: ModMed supports a handful of Primary Source Verification (PSV) integrations, but many practices still depend on manual credential checks due to incomplete API coverage or limited vendor support.
- Inconsistent state-level data exchange: Not all state medical boards provide standardized APIs, making automated verification inconsistent across regions and requiring manual intervention for certain credentials.
- Hospital committee requirements: Hospital credentialing bodies often request documentation formats that don’t align cleanly with ModMed’s EHR data outputs, creating additional administrative work.
- Supplementary credentialing tools: Some practices enhance ModMed’s native capabilities with third-party platforms like CAQH ProView or hospital-specific portals, creating a multi-system credentialing workflow.
- Data synchronization risks: Without a well-defined data flow protocol, synchronization issues can arise. For example, if Dr. Williams updates her malpractice insurance in CAQH, that update must be propagated back into ModMed’s provider file within a defined timeframe to maintain data accuracy and compliance.
Compliance Monitoring Beyond Basic Tracking
Credentialing automation should go beyond expiration alerts. ModMed’s reporting tools help administrators identify trends and potential risks early—such as clusters of upcoming renewals, facilities with unusual privileging delays, or CME patterns that hint at broader training needs.
For multi-location or multi-state practices, automated compliance monitoring is especially valuable, since manual tracking across diverse licensing rules is nearly impossible to maintain accurately.
The built-in audit trail is another major advantage during Joint Commission reviews or regulatory audits—it provides detailed verification logs that clearly show who reviewed each credential and when, eliminating last-minute compliance scrambles.
Real-World Implementation Lessons
When it comes to rolling out automation credentialing, this is not a technical implementation but rather a large workflow change for numerous departments. Success depends on solid change management and a dose of practicality when it comes to arranging the transition.
Start with data cleanup. Seriously. It is impossible to overemphasize the profound truth of this! It is counterproductive to attempt to automate credentialing without accurate and adequate baseline data. I would plan that you will spend a few weeks verifying our information against yours before putting any automated workflows in place.
Training requirements are quite different for different types of users. Doctors just have to learn how to update their own and respond to automatic requests. System administrators who possess a deep understanding of the system are needed to handle complex conditions and exceptions. The executive needs to have the reporting dashboard intuitiveness to oversee compliance at a high level.
The period of transition can be particularly tough. Deploying parallel manual and automated processes delivers a temporary safety belt but results in two of everything to manage. Between those two points is where most practices end as they roll out (first, very basic license tracking and then more sophisticated privileging workflows), which limits implementation anxiety.
Cost-Benefit Analysis in Practice
While credentialing automation requires upfront investment, the long-term efficiency gains easily justify the cost. Beyond saving time, it reduces compliance and operational risks—an expired credential or non-participating provider can be far more costly than the software itself.
Staff productivity also improves as teams focus on complex credentialing issues rather than routine renewals. Rather than cutting headcount, automation enhances precision—resulting in fewer billing errors, reduced scheduling conflicts, and smoother patient care continuity.
Looking Forward: Integration Opportunities
ModMed is still working on improving its credentialing features, but like many of its peers in the EHR world, it’s always making efforts to add new capabilities without compromising system stability. The primary room for improvement would be more extensive third-party verification and improving the predictive analytics capability of the tool.
Applications of artificial intelligence in credentialing are largely conceptual at this time but hold promise for pattern recognition and risk stratification. Think of systems that could predict which providers are likely to experience delays in renewal based on past behavior or even automatically spot deficiencies in an applicant’s credentials before they can affect a patient.








